Colorectal Cancer or Colon Cancer is one of the most common types of cancer, which initially begins with the abnormal growth of cells in the colon or rectum. This type of cancer typically doesn’t show significant symptoms in its early stages, and as a result, many individuals remain unaware of its existence until the disease has advanced. Regular screenings and monitoring risk factors can help in early detection and prevent its progression. Given the high prevalence and importance of prevention, recognizing the symptoms and treatment methods can significantly impact treatment outcomes and improve patients’ quality of life.
What is Colon Cancer and Colorectal Cancer?
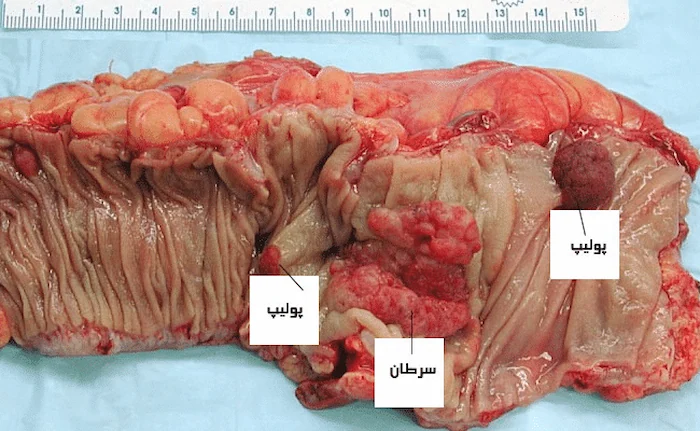
Colon cancer and colorectal cancer, which originate from the large intestine (colon) and rectum, are among the most common cancers of the digestive system. These cancers typically begin from precancerous polyps, which, due to genetic mutations, transform into abnormal cells. If not identified and treated, these cells can develop into cancer. Most colorectal cancers do not show clear symptoms in the early stages, which is why regular screening for the detection of polyps before they turn into cancer is crucial. Factors such as a family history of colon or rectal cancer, an unhealthy diet, alcohol consumption, and smoking are among the risk factors that increase the likelihood of developing these cancers. For the treatment of colon cancer, various methods such as surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy are available. According to the American Cancer Society, 1 in 22 men and 1 in 24 women may develop colorectal cancer during their lifetime.
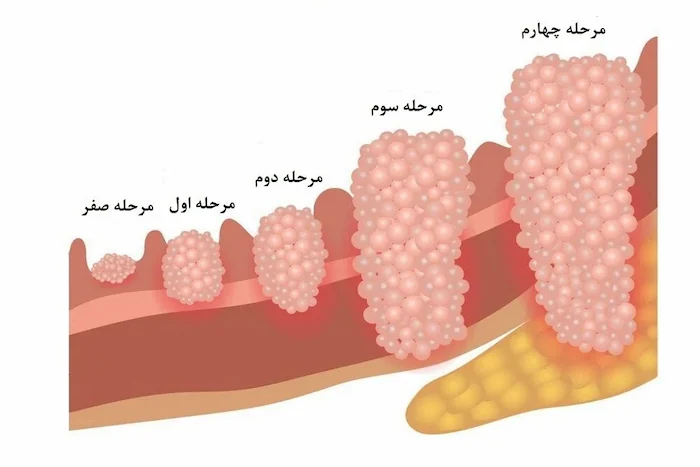
Stages of Colorectal Cancer Progression
The progression of colorectal cancer is typically assessed using a staging system, which helps determine the extent of the disease’s spread in the body. This system is used to identify the best treatment options and predict the course of the disease. Colorectal cancer can gradually spread from its initial stage, where it is confined to the inner lining of the large intestine, to other parts of the body. The different stages of cancer progression are explained as follows:
Stage 1: Tumor confined to the inner lining of the colon
In stage 1 of colorectal cancer, the tumor is confined to the inner lining of the large intestine, known as the “mucosa.” This stage represents the beginning of abnormal cell growth, but the tumor has not yet invaded the deeper layers of the colon. At this stage, the cancer has not spread to the lymph nodes or other organs of the body, and there is usually a high chance of successful treatment.
Stage 2: Invasion of the colon wall
In stage 2, the tumor has penetrated from the inner lining into the thick muscular layer of the colon and extends to the walls of the colon or rectum. However, at this stage, the cancer has not yet spread to the lymph nodes or nearby tissues. This stage typically indicates local spread of cancer, but the tumor has not yet metastasized to distant parts of the body.
Stage 3: Spread to lymph nodes
In stage 3, the cancer has crossed the wall of the colon and spread to the lymph nodes around the colon. The lymph nodes, part of the body’s immune system, act as natural filters and can also harbor cancer cells. Although the cancer has spread to the lymph nodes, it has not yet spread to other parts of the body. Treatment at this stage may involve surgery, chemotherapy, and radiotherapy.
Stage 4: Spread to other parts of the body
Stage 4 colorectal cancer is the most advanced stage, where the tumor has spread to distant organs such as the liver or lungs. This stage is commonly known as metastasis, where cancer cells break away from the primary site and spread to other parts of the body. Treatment at this stage is typically more challenging and may involve advanced therapies such as chemotherapy, immunotherapy, and targeted therapy.
Read more: Everything you need to know about oncology | Best Oncology Clinic in Golestan
Types of Colorectal Cancer
Although colorectal cancer is generally recognized as a single type of cancer, in reality, there are various types of this cancer, each differing based on the type of cancerous cells and their location in the body. Each of these types has its own unique characteristics, which impact the diagnosis and treatment process.
Adenocarcinomas
The most common type of colon cancer, adenocarcinomas, accounts for about 96% of colon cancer cases. This type of cancer forms in the mucus-producing cells of the colon or rectum and is generally recognized as the predominant type of colorectal cancer. These tumors arise from glands in the inner lining of the colon or rectum and are considered the primary type when diagnosing colorectal cancer.
Lymphomas
Lymphomas may initially form in the lymph nodes or in the colon. This type of cancer originates from the immune system cells and may gradually spread to the colon. Lymphomas are generally not common in the digestive system, but in some cases, they can be observed in the colon.
Read more: What is Lymphoma? | Types | Diagnosis and Treatment Methods
Carcinoids
Carcinoids are a type of tumor that begins in the hormone-producing cells in the large intestine. These tumors usually grow slowly and may not produce any symptoms in the early stages. In some cases, these tumors may respond to hormones and can cause symptoms such as flushing or hormonal issues.
Sarcomas
Sarcomas typically form in soft tissues such as the muscles of the colon. These cancers begin in connective tissue cells and are less common than other types of colorectal cancer. Sarcomas may present symptoms similar to those of other colon cancers but require specific methods for diagnosis.
Gastrointestinal Stromal Tumors (GISTs)
Gastrointestinal stromal tumors usually begin in the connective tissue cells of the digestive system. These tumors can initially be benign, but in some cases, they may develop into cancer. Although these tumors are more common in the stomach or small intestine, they can occasionally occur in the colon as well, though this type of colorectal cancer is rare.
Early Symptoms of Colorectal Cancer:
- Constipation
- Diarrhea
- Change in stool color
- Change in stool shape (such as narrowing of stool)
- Presence of blood in the stool
- Rectal bleeding
- Excessive gas production
- Abdominal cramps
- Abdominal pain
Symptoms in Advanced Stages of Colorectal Cancer:
- Extreme fatigue
- Unexplained weakness
- Unintentional weight loss
- Changes in bowel movements lasting more than a month
- Feeling that the bowel is not completely empty
- Vomiting
Symptoms of Cancer Spreading to Other Parts of the Body:
- Jaundice (yellowing of the eyes and skin)
- Swelling in the hands or feet
- Breathing difficulties
- Chronic headaches
- Blurred vision
- Bone fractures
- Gastrointestinal bleeding

Causes of Colorectal Cancer:
Researchers are still studying the exact cause of colorectal cancer. However, various factors—both direct and indirect—contribute to the development of colorectal cancer, often interacting with one another.
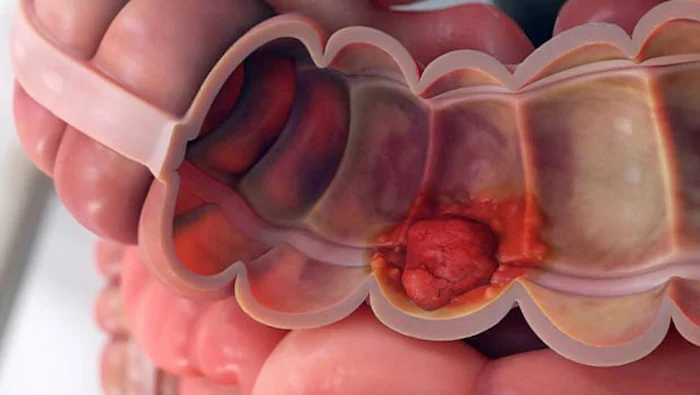
Pre-cancerous Growths
Abnormal cells that accumulate in the lining of the colon lead to the formation of polyps. Polyps are benign clusters of cells that, if left untreated, can become cancerous. One of the preventive measures for colorectal cancer is the removal of these polyps through surgery.
Genomic Mutations
Sometimes, colorectal cancer runs in families. This is due to mutations in specific genes that are inherited and passed down through generations. These genetic mutations increase the likelihood of developing colorectal cancer, although they do not necessarily guarantee that it will occur.
Read More: Genetic Testing for Hereditary Cancers
Who is at Risk for Colorectal Cancer?
Non-modifiable Factors
Some factors that increase the risk of colorectal cancer are unavoidable, including:
- Age: The risk of developing colorectal cancer increases after the age of 50.
- History of Colon Polyps: Individuals who have previously had colon polyps are at a higher risk.
- History of Inflammatory Bowel Diseases: Diseases such as Crohn’s disease or ulcerative colitis can increase the risk of colorectal cancer.
- Family History of Colorectal Cancer: A family history of colon or rectum cancer increases the risk.
- Genetic Syndromes: People with specific genetic syndromes, such as familial adenomatous polyposis, are more likely to develop colorectal cancer.
- Ethnicity: People of Eastern European Jewish or African descent are at higher risk for colorectal cancer.
Modifiable Factors
There are also several factors that can be changed to reduce the risk of colorectal cancer. These are preventable and include:
- Overweight or Obesity: Obesity increases the risk of colorectal cancer.
- Tobacco Use: Smoking is a major risk factor for colorectal cancer.
- Excessive Alcohol Consumption: Drinking too much alcohol can increase the risk of colorectal cancer.
- Type 2 Diabetes: People with type 2 diabetes are at greater risk for colorectal cancer.
- Physical Inactivity: Lack of physical activity increases the risk of colorectal cancer.
- Poor Diet: A diet high in fat, low in fiber, processed foods, and high in red meat, while low in fruits and vegetables, can increase the risk of colorectal cancer.
Screening Tests and Diagnostic Methods for Colorectal Cancer
Early detection of colorectal cancer is crucial as it can significantly increase the chances of recovery. Doctors use various methods for diagnosing this cancer, and some of them are outlined below:
Fecal Immunochemical Test (FIT)
This test detects hidden blood in the stool. Blood vessels in polyps or larger cancers are often fragile and can be easily damaged, releasing blood into the stool.
Fecal DNA Test
Colorectal cancer cells or polyp cells often have genetic mutations in specific genes. These cells enter the stool, and this test examines the stool for genetic mutations and markers.
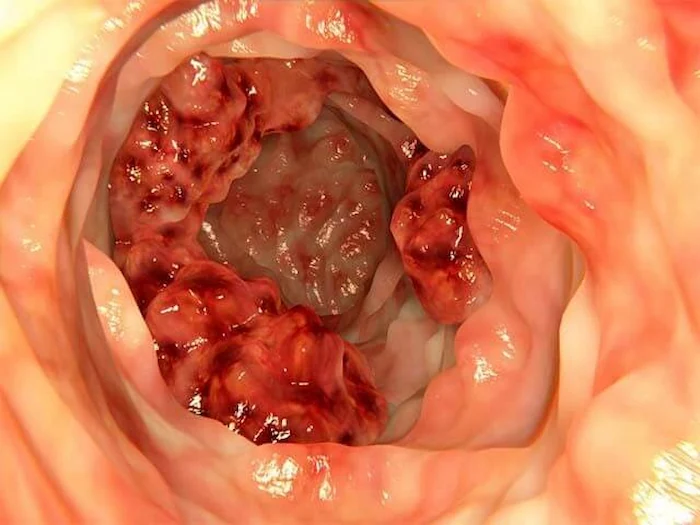
Colonoscopy
In this method, a doctor uses a long tube with a camera to view the inside of the colon and rectum. Any abnormal areas are examined, and biopsies may be taken if necessary.
CT Colonography (Virtual Colonoscopy)
This advanced method of CT scanning uses X-rays to capture images of the colon and rectum. It’s a non-invasive way to check for abnormalities in the colon.
Clinical Tests and Biopsy
The doctor may perform blood tests and a physical examination. If a suspicious polyp or lesion is found during the examination, a biopsy is done, and a tissue sample is sent to the lab for further analysis.
X-ray Imaging
The doctor might use X-ray imaging. In this method, a barium contrast solution is introduced into the colon through an enema, coating the colon lining to provide clearer images.
CT Scan
This method is used to create detailed images of the colon and is also referred to as virtual colonoscopy. The CT scan helps doctors identify any issues or growths within the colon.

When Should You See a Gastroenterologist for Colorectal Cancer Diagnosis?
Given the serious risks associated with colorectal cancer and its difficulty in being detected at early stages, it is recommended to undergo regular screening tests. Especially if you are 50 years old or older and at average risk for colorectal cancer, screenings such as annual fecal occult blood tests, flexible sigmoidoscopy (every 5 years), and colonoscopy (every 10 years) are advised.
Which Doctor Should You See for Colorectal Cancer Diagnosis and Treatment?
To diagnose and treat colorectal cancer, it’s best to first consult with an internist who specializes in gastrointestinal diseases. If initial treatments by the internist do not yield positive results, the patient will be referred to a gastroenterology, liver, and endoscopy subspecialist.
Best Colorectal Cancer Treatment Clinic in Gorgan
If you’re seeking colorectal cancer treatment in Gorgan, Shafa Clinic is one of the best treatment centers in the area. With expert specialists in cancer care, including colorectal cancer, and advanced equipment and modern treatment methods, Shafa Clinic offers comprehensive and complete services. Patients at Shafa Clinic can benefit from specialized consultations and thorough follow-ups to ensure the best possible treatment outcomes.
Treatment Methods for Colorectal Cancer
The treatment of colorectal cancer depends on various factors, including the stage of the disease and the general health of the patient. Below are some common treatment methods for colorectal cancer:
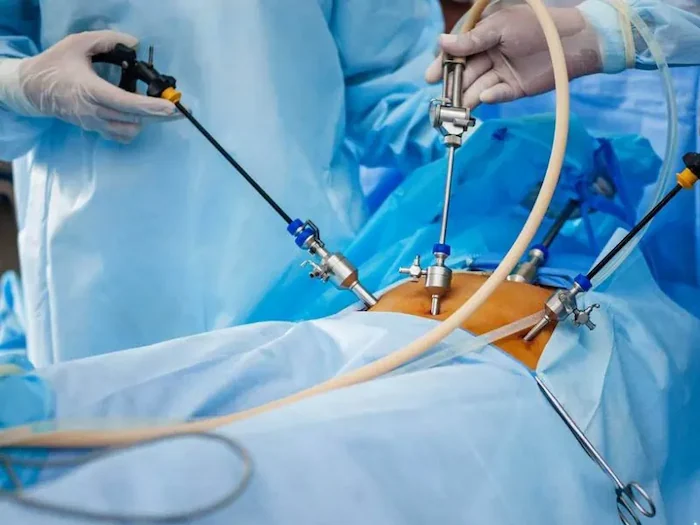
-
Surgery In the early stages of cancer, surgery to remove the tumor is performed. If the cancer has not spread to the colon wall, surgery is generally successful. If the cancer has spread, sections of the colon or rectum and nearby lymph nodes may be removed. In some cases, a colostomy (creating an opening in the abdominal wall) may be required.
-
Chemotherapy Chemotherapy uses anti-cancer drugs systemically to kill cancer cells. It is usually applied after surgery to eliminate any remaining cancer cells. Chemotherapy may also be used to shrink tumors before surgery.
-
Radiation Therapy Radiation therapy uses high-energy rays to destroy cancer cells. This method is often combined with chemotherapy and is beneficial in cases where cancer cells are concentrated in specific areas of the body.
-
Targeted Therapy Targeted therapies, such as regorafenib (Stivarga), are used for treating advanced cancer that does not respond to other treatments. These drugs work by blocking enzymes that stimulate the growth of cancer cells.
-
Immunotherapy Immunotherapy uses the body’s immune system to fight cancer. It involves stimulating the immune system with specific proteins or compounds to enhance the body’s response.
-
Other Methods Additional treatments like heat therapy, cryotherapy, stem cell transplants, and drugs like Avastin and Glioc are considered for managing the disease in advanced stages.
Complications of Colon Cancer
After colon cancer treatment, individuals may experience certain complications that improve over time. To better manage these complications, it is important to consider the following:
1. Changes in Bowel and Sexual Function:
After colon cancer surgery, changes in bowel and bladder function may occur. These issues usually improve within the first few months, but in some cases, the process may take longer. Erectile dysfunction is particularly common after rectal cancer surgery.
2. Fatigue:
Feeling fatigued after surgery is normal. Light exercise and following the doctor’s recommendations can help improve the condition, but the individual may feel easily tired and require more rest. Rest and limitations, such as avoiding heavy lifting, can be helpful.
Prevention of Colon Cancer
To reduce the risk of colon cancer, it is essential to follow these guidelines:
- Reduce consumption of red and processed meats.
- Increase intake of plant-based foods.
- Reduce unnecessary fat consumption.
- Exercise regularly and maintain a healthy weight.
- Quit smoking and reduce alcohol consumption.
- Manage stress and control diabetes.
- Undergo colonoscopy starting at age 50 for early detection.
Long-Term Outlook for Colorectal Cancer Patients with Early Diagnosis
If colorectal cancer is diagnosed in its early stages, the success rate of treatment and recovery is high. Patients with early-stage disease, if treated appropriately and without recurrence, can live healthily for 5 years or more. This significantly improves the life outlook for patients.


No comment